Journal of Multidisciplinary Studies in Human Rights & Science (JMSHRS)
Volume 7, Issue 5, Special Issue on Deflection - IV - 2025 | SDGs: 3 | 5 | 10 | 16 | #RethinkProcess ORIGINAL SOURCE ON: https://knowmadinstitut.org/journal/
DOI: 10.5281/zenodo.15223938
Volume 7, Issue 5, Special Issue on Deflection - IV, April 2025 | SDGs: 3 | 5 | 10 | 16 |
DOI: 10.5281/zenodo.15223938
What It Takes:
Implementation and Expansion of a Quick Response Team
Sarah M. Manchak, Ph.D.*
Sarah Light, M.S.
Madeline Lancaster, M.S.
- Institute of Behavioral Research, Texas Christian University. ORCID: -Unknown-
Bradley O’Guinn, M.S.
Meagan Guthrie, M.A.
- Hamilton County Ohio Office of Addiction Response. ORCID: -Unknown-
Cory Haberman, Ph.D.
EN | Abstract:
Quick Response Teams (QRTs) have proliferated across the United States in response to the opioid overdose crisis. One of the first county-wide QRTs in the nation, the Hamilton County, Ohio QRT (HC-QRT), has been heralded as a model QRT, and its members have helped to train and teach other jurisdictions wishing to implement similar programs. This is the first of several studies of this QRT’s operations. The present study describes and quantifies the HC-QRTs activities and outputs as it has expanded over a seven-year period.
Key Words: Deflection, Quick Response Teams, Opioid, Outreach, Substance Use, Addiction, Overdose Response, Community Safety, Criminal Justice, SDG 1, SDG 3, SDG 5, SDG 10, SDG 16, SDG.
ES | Abstract:
Los Equipos de Respuesta Rápida (QRT, por sus siglas en Ingles) han proliferado por todo Estados Unidos en respuesta a la crisis de sobredosis de opiáceos. Uno de los primeros QRT a escala de condado del país, el QRT del condado de Hamilton, Ohio (HC-QRT), ha sido anunciado como un QRT modelo, y sus miembros han ayudado a formar y enseñar a otras jurisdicciones que desean implantar programas similares. Este es el primero de varios estudios sobre el funcionamiento de este QRT. En el presente estudio se describen y cuantifican las actividades y los resultados de HC-QRT a medida que se ha ido ampliando durante un período de siete años.
Palabras clave: Deflexión, equipos de respuesta rápida, opiáceos, divulgación, consumo de sustancias, adicción, respuesta a sobredosis, seguridad comunitaria, justicia penal, ODS 1, ODS 3, ODS 5, ODS 10, ODS 16, ODS.
INTRODUCTION
The opioid overdose epidemic has ravaged communities throughout the nation, costing over 725,000 lives between 1999 and 2022. The state of Ohio has been among the hardest hit states, with over 35,000 unintentional overdose deaths due to opioids between 2014 and 2023 (Ohio Department of Health, 2023). As overdose and overdose deaths began to spike with the advent of synthetic opioids, it became apparent that something different from the status quo needed to be done. Too many people were dying, and the traditional ways in which communities were responding to substance use disorder (SUD)—with stigma, criminalization, and placing the onus on individuals struggling with SUD to seek out treatment and support on their own—was simply not working. In fact, it may have been making the crisis even worse.
With crisis often comes opportunity and innovation, and one program that developed in the summer of 2015 in Colerain Township, Ohio offered a completely new approach to addressing overdoses in the Cincinnati area. A Quick Response Team (QRT) was formed from a partnership between law enforcement, mental health and addiction service providers, and peer support specialists. Several days a week, a small team of individuals representing these disciplines went out into the community, knocking on doors of individuals who recently experienced a nonfatal overdose, offering resources, support, and help connecting people to treatment.
As time went on, word of the success of this team spread quickly, and many jurisdictions throughout Ohio began to replicate the model in their own communities. In so doing, these QRTs were molded in response to their own community’s unique needs and in a way that each team’s resources and environment could support.
THE HAMILTON COUNTY QUICK RESPONSE TEAM: INITIAL IMPLEMENTATION
In 2017, Hamilton County, Ohio, the county that incorporates Colerain Township and the city of Cincinnati and its surrounding area, began a county-wide QRT with the support of funds from the Bureau of Justice Assistance (BJA) “Comprehensive Opioid Site-Based Program” (COAP) grant. This QRT, which operated two days a week—one day on the East side of Cincinnati and one day on the West side—was led by the Commander of the Heroin Task Force—an entity that was responsible for investigating and bringing to justice drug dealers linked to opioid overdoses in the city. He was joined by a licensed behavioral health and addiction treatment professional and two individuals with lived experience in active recovery.
On their designated days, the team would meet first thing in the morning and review a list of names of individuals from calls for service data who had recently had a nonfatal overdose. With law enforcement intelligence gathered by the Hamilton County Fusion Center, an entity originally created to provide a centralized and streamlined way to gather and communicate information relevant to public safety in the county, the team was able to plan their day.
They mapped out the route they would take to visit the homes of individuals who recently overdosed, and they came equipped with phone numbers, email addresses, and even social networking handles for these individuals, as well as their next of kin.
The team then set forth, driving in their QRT-marked vehicle and clad in QRT-branded polo shirts and khakis, going house to house, neighborhood to neighborhood, knocking on doors, and asking “how can we help?” They offered resources, educational materials, and later, harm reduction supplies (e.g., naloxone and fentanyl test strips[1]). In some instances, the team helped individuals reconnect with providers they already had, accompanied them to an NA or AA meeting, or called treatment facilities to set up assessments.
In other instances, the team transported individuals directly to the Hamilton County Engagement Center, a short-term triage treatment facility run by a local nonprofit agency called Talbert House, which aided in detoxification and withdrawal support, initial case management, and linkage to longer-term SUD care.
If an individual was not interested in treatment, resources would be left behind and the QRT would emphasize that the door is always open for the person to change their mind and reach out. Oftentimes, the team would engage with the loved ones of the person who experienced an overdose and offer them resources for support as well. In some instances, family members or friends of the person the QRT visited would also be interested in receiving treatment themselves.
EXPANSION OF THE HAMILTON COUNTY QUICK RESPONSE TEAM
Over time, the Hamilton County Quick Response Team grew into a full-time deflection program that now currently operates on all six identified (BJA, 2023) deflection pathways and with oversight from the Hamilton County Office of Addiction Response. However, between its initial implementation as a two-day per week reactive overdose response model and its full-time current implementation as a six-pathways deflection program, it expanded to a full-time overdose response + proactive targeted outreach model that was supported by a variety of funding streams at different time points (see Table 1 and Acknowledgements).
This expanded QRT model now included proactive outreach in four core areas: (a) “hot spot” neighborhoods hardest hit by overdose, where neighborhood canvassing and outreach took place; this later morphed into targeted outreach to people who were high service utilizers and/or responsible for repeat police calls for service (Holistic Outreach to Priority People, or HOPP); (b) the county justice center, where primarily Naloxone distribution took place, (c) with the county drug treatment and recovery court docket (DTRC), where a peer navigator was embedded to support and assist court clients; and (d) among the county’s Black and African American population, which had recently experienced disproportional uptick in overdoses (Hamilton County Public Health, 2024). Additionally, overdose response activities shifted to fulltime—Monday through Friday during normal work hours, beginning in October 2020. The intent of all four of these proactive targeted outreach efforts was to provide education, resources, peer support, treatment referrals and connection, and harm reduction supplies in areas and to the people who needed them most.
BUILDING AN EVIDENCE BASE IN HAMILTON COUNTY AND BEYOND
Since their inception, researchers have faced myriad challenges studying QRTs, which has, in turn, contributed to a rather slow roll out of evidence on their effectiveness (Manchak et al., 2024). Implementation of QRTs has historically been quite idiosyncratic, and there is wide heterogeneity in team composition, scope, and activities (Bailey et al., 2023; Formica et al., 2018). Furthermore, QRTs do not yet operate using universally standardized language for their outputs. Referrals to treatment and connections to care are operationalized differently. Even the word “treatment” itself means something different for every client served, as one key value that drives QRT efforts is to meet individuals where they are and provide them with what they need in the moment.
Due to the varied ways in which QRTs are implemented, much of what is empirically known to date about QRTs is largely descriptive, and evaluation studies examine a wide range of outcomes (see Ferg et al., 2024). Moreover, only a few known studies have attempted to identify how aspects of the QRT process (e.g., referral source, frequency and timing of contact) relate to client outcomes (Collins et al., 2021; Dahlem et al., 2021; Formica et al., 2021; Kimmel et al., 2023; Ray et al., 2023). T
his paper seeks to contribute to the literature on QRTs, leveraging the data and experiences of the Hamilton County Quick Response Team (HC-QRT), a QRT that has been heralded as a model QRT in the field, both because of its size and sheer volume of individuals served, but also because of its organization and implementation success.
In close partnership with a team of researchers, the HC-QRT has been able to develop a replicable logic model, standardized language surrounding the logic model components, and systematic data collection to facilitate a robust descriptive assessment of HC-QRT’s outputs and client outcomes.
The present study has one primary aim: to quantify outputs of the HC-QRT over a seven- year period of implementation and expansion. To address this aim, we present summary descriptive statistics for HC-QRT outputs and client outcomes from initial implementation as a part-time overdose response model to a full-time, multi-pathway model.
METHOD
Setting
Hamilton County spans a total of 413 square miles of southwestern Ohio. According to the U.S. Census Bureau in 2023, 827,058 people resided in the county. Just over half of those residents were female (51.4%). White individuals made up the majority of the county population at just over 67%, followed by Black or African American (26.6%), and Hispanic or Latino (4.9%). In 2021, Hamilton County Public Health reported 2,591 overdose emergency department visits, compared to 2,046 in 2022, and less than 2,000 in 2023. Additionally, the number of overdose deaths has also steadily decreased since 2017. In 2017, a reported 444 residents died of drug overdoses in Hamilton County, whereas a reported 366 died in 2020, and 333 in 2023. There were 32.6 overdose deaths per 100,000 people nationally in 2022 (CDC, 2024), compared to 41.3 overdose deaths per 100,000 in Hamilton County (Ohio Department of Health, 2023).
Measures
The constructs examined in this study are part of the HC-QRT logic model and listed in Table 2 in greyscale and defined below. For the purposes of clarification, activities are operationalized below though, but only the outputs of these activities are measured and examined in the current study.
Activities of the QRT during the period that this study examines are (1) overdose response (door knocks and outreach to individuals who recently had a nonfatal overdose to offer treatment and support), (2) harm reduction distribution (Naloxone was distributed at the county jail, during community outreach events, and during individual one-on-one interactions), (3) community outreach (formal outreach events, often in partnership with other social or substance use awareness events), (4) targeted outreach (canvassing in neighborhoods that are hardest hit by overdoses and overdose deaths, Black/African American targeted outreach, and peer navigation at the justice center and the drug treatment and recovery court), (5) education (included one-on-one discussion about Naloxone and how to administer it and provision of information about community resources and safe use practices), (6) peer support (delivered in a variety of settings and included ongoing social/emotional support and resource/referral navigation assistance), and (7) referrals and connections to care.
Outputs
The indices of outputs include (1) total number of community outreach events, (2) total number of miles traveled, (3) total number of team engagements and transports to treatment. (4) total harm reduction supplies distributed, (3) total number of unique individuals successfully engaged with who recently experienced a non-fatal overdose, (5) total number of unique targeted outreach clients successfully engaged, (6) total number of successful follow up engagements with any QRT clients, after the initial engagement.
Outcomes
Individual-level outcomes can be both short-term/proximal and long-term/distal. This study focuses only on short-term outcomes, as the long-term outcome data is not yet available. Short term outcomes include (1) successful engagement, defined as actual physical or verbal contact with the individual, and (2) referral or connection to treatment, defined as a formal referral or warm hand off to a provider or agency.
Procedures
Output and outcome data were routinely entered into a case management software database that was designed specifically to meet the QRT needs. Typically, peer navigators entered information about client contacts in real-time (or close to real time) using a tablet while conducting work in the field or follow-up work from the office or home. These data were later extracted and analyzed by the evaluation team. Navigators recorded the date of referral, date of all interaction attempts, the route of interaction attempts (phone, face-to-face, email/social media), whether the interaction was successful or not (i.e., engagement took place between the two parties), and when a resolution occurred (referral or connection to treatment), the appropriate short-term outcomes. Additionally, team-based QRT outputs—specifically the total number of miles driven to reach individuals, total clients transported, total individuals engaged and transported to treatment, and total number of outreach events were tracked using an “officer daily” log, which was submitted to the evaluation team on a regular basis for data entry and analysis.
RESULTS
IMPLEMENTATION OF QRT ACTIVITIES AND OUTPUTS
COMMUNITY OUTREACH EVENTS
From November 2021 through Sept 2024, the HC-QRT conducted a total of 1, 220 community outreach events, taking place at a variety of locations including the jail, mobile outreach buses, several YMCAs, Churches, food kitchens, libraries, neighborhoods, and local markets.
MILES TRAVELED
In a given shift, The QRT could travel anywhere between 3 and 157 miles. On average, the QRT traveled 60 miles per shift (SD = 25). When the QRT was a part time overdose response program, the team would travel on average of 74 miles per shift (SD = 26), but this dropped to an average of 55 miles per shift (SD = 23) once it became a full-time, five-days-per-week model. Notably, mileage data is available for only 65% of part-time QRT and 33% of full- time QRT reported shifts.
TEAM ENGAGEMENTS AND TRANSPORTS TO TREATMENT
Over the seven-year implementation and expansion period, QRT shift reports indicate that the HC-QRT made 0 to 66 face-to-face interactions per shift. About 50% of shifts included face-to-face interactions with 0,1,2,3, or 4 individuals. Additionally, QRT shift reports indicate that a total of 261 individuals were directly transported to treatment during this time, with anywhere from 0 to 10 people transported to treatment in a given shift. After zero, the modal number of clients transported per shift was 1. Notably, almost half (45%) of QRT shift reports are missing transportation data.
HARM REDUCTION MATERIALS DISTRIBUTED
In any given shift, the QRT distributed up to 36 Naloxone kits, 81 fentanyl test strips, and 51 hygiene packs. On average, the team distributed 3.5 (SD = 4.5) Naloxone kits, 3 (SD = 7) fentanyl test strips, and 4 (SD = 6) hygiene packs per shift. Between September 2020 and September 30, 2024, The QRT distributed a total of 3,821 Naloxone kits.
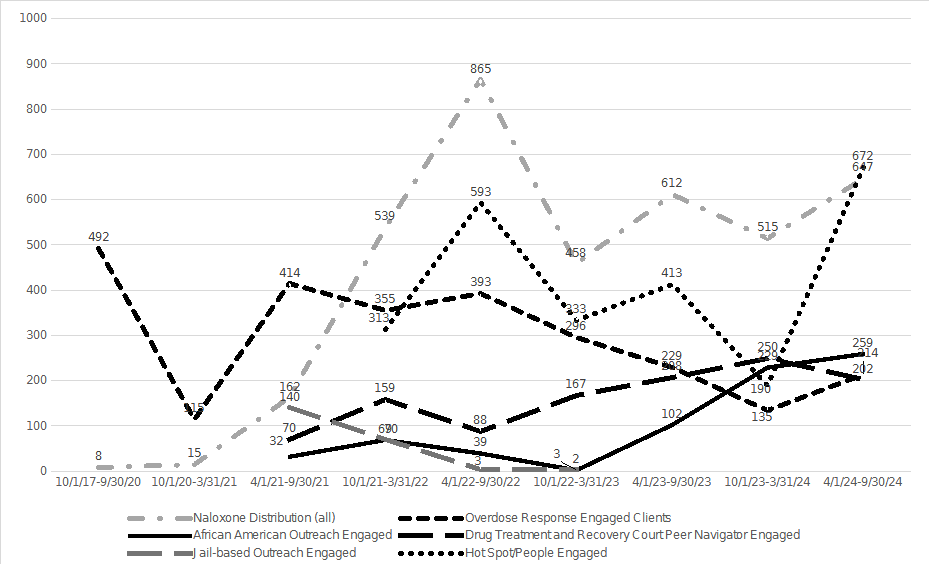
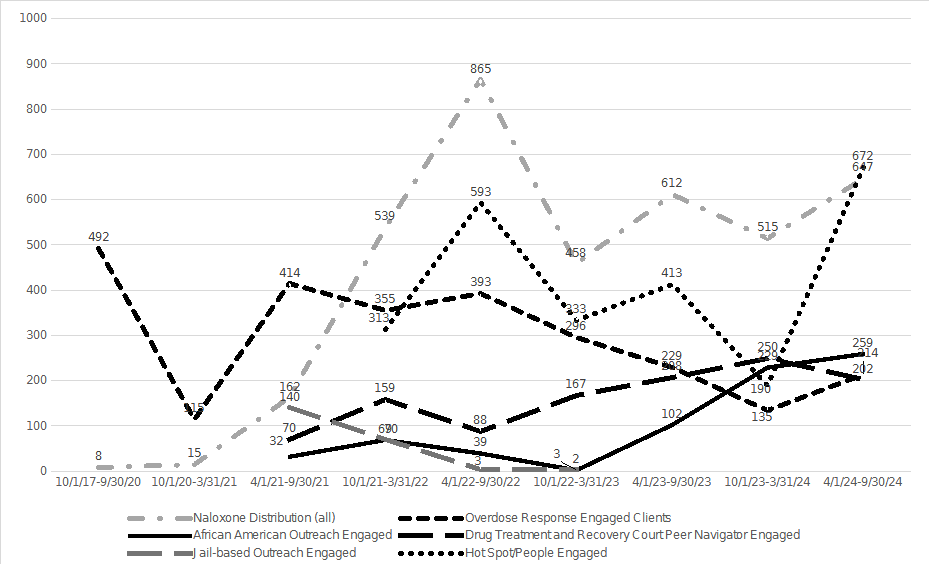
INDIVIDUALS TARGETED AND ENGAGED
In total, the QRT attempted engagement with 7,247 individuals[2] across the five different routes of engagement: overdose response clients (n = 2,643); African American targeted outreach clients (n = 732); justice center targeted outreach clients (n = 216); hotspot/HOPP targeted outreach clients (n = 2,514); and drug treatment and recovery court clients (n = 1,142). Of the 7,247 individuals for whom the QRTs attempted contact, 5,436 were successfully engaged/contacted (75%): overdose response clients (n = 1,127); African American targeted outreach clients (n = 573); justice center targeted outreach clients (n = 201); hotspot/HOPP targeted outreach clients (n = 2,410); and drug treatment and recovery court clients (n = 1,125).Of those successfully engaged, 1,060 individuals continued to have successful, ongoing engagement (19.5%). Across the five routes of engagement, the QRT had 9,170 successful interactions with clients and were able to refer or connect 615 unique individuals to treatment (11.3% of those successfully engaged with/contacted). Table 3 provides these metrics broken down by each route of engagement.
DISCUSSION
This study is among a small cohort of extant studies describing QRTs and other overdose response programs. In contrast to prior studies of this nature, which more qualitatively describe the components of program implementation (Canada & Formica, 2022; Carroll et al., 2023; Collins et al., 2021; Formica 2022; Formica et al., 2021; Powell et al., 2019; Senthilkumar et al., 2023), this study quantified implementation activities. Similar to Ulintz and colleagues (2024), also an Ohio-based team, our findings are presented over an extended period of time of implementation, offering a realistic picture of “what it takes” to implement a QRT in a larger Midwestern urban county. Several insights can be gleaned by examining the trends of the HC-QRT engagement activities over time.
First, this study demonstrates how resources (e.g., grant funding) and capacity (e.g., fully staffed team and full-time operations) allow for increased engagement with individuals struggling with substance use. As the QRT transitioned into a full-time model, their capacity to reach more people increased, but there also was a clear demand for these increased QRT services. That substantially more people were reached as the model expanded, suggests that this is a full-time response requiring full-time resources.
Second, as the QRT began to engage in proactive targeted outreach, there was a noticeable decline in overdose response cases. This was not a function of lack of resources to do overdose response work; the QRT continued to make contact attempts in the exact same way, following the exact same protocols as before it transitioned to an expanded model (i.e., working from EMS/Fire, law enforcement, and emergency department overdose lists). While causality cannot be established in this case, it is quite possible that the proactive targeted outreach, coupled with widespread Naloxone distribution, may have resulted in less need for overdose response.
Third, the rate of successful engagement—75%--out of attempted contacts is quite remarkable. Of course, this figure may be buttressed by the success of targeted outreach work, but even among just overdose response clients, the QRT was able to successfully engage with almost half (43%) of those referred to the team. Individuals who use substances are historically a difficult population to engage, in part because they are difficult to locate (Cunningham et al., 2008) and have high rates of homelessness and transience (Ferguson et al., 2014; McVicar et al., 2015). The successful engagement rate by the HC-QRT is a testament to their persistence and willingness to do what is necessary to find and connect with individuals struggling with substance use.
Fourth, referral and connection to treatment outcomes, in comparison to successful engagement, are significantly lower. On the face of it, such a low yield may be interpreted as unsuccessful, but it is important to contextualize these data. The rates of treatment engagement for people with SUD generally are quite low and have been consistently so over time (see Liu et al., 2020; Sakher et al., 2024; Office of the Surgeon general, 2016; Substance Abuse and Mental health Services Administration 2015). Studies have proffered many reasons for this trend, including stigma (Benz et al., 2021, Hammarlund et al., 2018), lack of insurance (Ali et al., 2015; Feder et al., 2019; Haughwout et al., 2016), and disparate access to resources (Lu et al., 2023). While we were unable to measure these constructs in the current study, the varied functions of the QRT serve to remove these types of barriers for people with SUD. In so doing, the individuals the QRT serves may, as a result, have greater ability to eventually engage in treatment than they would have, if not for their interactions with the QRT. Moreover, the fact-paced, high-volume operations of the QRT do not allow for ongoing tracking of client outcomes. As such, the referral/connection to treatment outcome, which reflects the QRT’s awareness of an outcome at the time of their interaction (which is short-lived), is likely an underestimate of what eventually takes place with the individuals served.
The study findings contribute to a growing literature on QRTs and other deflection programs. Quantifying outputs in the manner done in this paper allows for other jurisdictions to get a realistic understanding of what day-to-day operations entail. However, the findings must also be understood in context. The HC-QRT operates in a highly unique environment, which may not be replicable in other jurisdictions. Hamilton County is a rather resource-rich county.
Furthermore, as the QRT developed, so did a very large cadre of agencies and entities that grew in size and collaborative spirit over time, culminating in the creation of a formal Addiction Response Coalition, which meets monthly, and the creation of an entire Addiction Response Agency that oversees the county’s interdiction, prevention, and intervention efforts.
The infrastructure supporting the QRTs efforts is strong, and community partnerships create increased opportunity for the QRT to be successful. Jurisdictions wishing to emulate programs such as the HC-QRT must be aware of the crucial importance of traditional divers of program implementation (see Glasgow et al., 2024).
REFERENCES
- Ali, M. M., Teich, J. L., & Mutter, R. (2015). The role of perceived need and health insurance in substance use treatment: Implications for the Affordable Care Act. Journal of Substance Abuse Treatment, 54, 14-20.
- Bailey, A., Harrington, C., & Evans, E. A. (2023). A scoping review of community-based post-opioid overdose intervention programs: implications of program structure and outcomes. Health and Justice, 11(1), 3.
- Benz, M. B., Cabrera, K. B., Kline, N., Bishop, L. S., & Palm Reed, K. (2021). Fear of stigma mediates the relationship between internalized stigma and treatment-seeking among individuals with substance use problems. Substance Use and Misuse, 56(6), 808-818.
- Blevins, C. E., Rawat, N., & Stein, M. D. (2018). Gaps in the substance use disorder treatment referral process: Provider perceptions. Journal of Addiction Medicine, 12(4), 273–277.
- Bureau of Justice Assistance. (2023). The Six Pathways: Frameworks for Implementing Deflection to Treatment, Services, and Recovery. https://www.cossup.org/Content/Documents/Articles/CHJ-TASC_Six_Pathways_Framework_for_Implementing_Deflection_June_2023.pdf
- Center for Disease Control. (2024, November 1). Understanding the Opioid Overdose Epidemic. https://www.cdc.gov/overdose-prevention/about/understanding-the-opioid-overdose-epidemic.html
- Cunningham, R., Walton, M. A., Tripathi, S. P., Outman, R., Murray, R., & Booth, B. M. (2008). Tracking inner city substance users from the emergency department: how many contacts does it take? Academic Emergency Medicine, 15(2), 136-143.
- Feder, K. A., Krawczyk, N., Mojtabai, R., Crum, R. M., Kirk, G., & Mehta, S. H. (2019). Health insurance coverage is associated with access to substance use treatment among individuals with injection drug use: Evidence from a 12-year prospective study. Journal of Substance Abuse Treatment, 96, 75-81.
- Ferg, M., Rapisarda, S. S., Soranno, E., Lewis, N., Ottoson, A., & Tschampl, C. A. (2024). Bridging the gap: An environmental scan of post-overdose program features and evaluation measures. International Journal of Drug Policy, 134, 104651.
- Ferguson, K. M., Bender, K., & Thompson, S. J. (2014). Predictors of transience among homeless emerging adults. Journal of Adolescent Research, 29(2), 213-240.
- Formica, S. W., Apsler, R., Wilkins, L., Ruiz, S., Reilly, B., & Walley, A. Y. (2018). Post opioid overdose outreach by public health and public safety agencies: Exploration of emerging programs in Massachusetts. International Journal of Drug Policy, 54, 43-50.
- Glasgow, R. E., Trinkley, K. E., Ford, B., & Rabin, B. A. (2024). The Application and evolution of the Practical, Robust Implementation and Sustainability Model (PRISM): History and innovations. Global Implementation Research and Applications, 4(4), 404-420.
- Hamilton County Public Health. (2024). Monthly Fatal overdose. https://hamiltoncountyhealth.org/monthly-fatal-overdose-report/
- Hammarlund, R., Crapanzano, K. A., Luce, L., Mulligan, L., & Ward, K. M. (2018). Review of the effects of self-stigma and perceived social stigma on the treatment-seeking decisions of individuals with drug-and alcohol-use disorders. Substance Abuse and Rehabilitation, 115-136.
- Haughwout, S. P., Harford, T. C., Castle, I. J. P., & Grant, B. F. (2016). Treatment utilization among adolescent substance users: Findings from the 2002 to 2013 National Survey on Drug Use and Health. Alcoholism: Clinical and Experimental Research, 40(8), 1717-1727.
- Kimmel, S. D., Xuan, Z., Yan, S., Lambert, A. M., Formica, S. W., Green, T. C., ... & Walley, A. Y. (2023). Characteristics of post-overdose outreach programs and municipal-level opioid overdose in Massachusetts. International Journal of Drug Policy, 120, 104164.
- Liu, J., Storfer-Isser, A., Mark, T. L., Oberlander, T., Horgan, C., Garnick, D. W., & Scholle, S. H. (2020). Access to and engagement in substance use disorder treatment over time. Psychiatric Services, 71(7), 722-725.
- Lu, W., Xu, L., Goodwin, R. D., Muñoz-Laboy, M., & Sohler, N. (2023). Widening gaps and disparities in the treatment of adolescent alcohol and drug use disorders. American Journal of Preventive Medicine, 64(5), 704-715.
- Manchak, S. M., Light, S., Strange, C. C., Farringer, A., Firesheets, K., Kirven, J., Ross, J., Juarez, S., & Sperber, K. G. (2024). Current trends and future directions for building the evidence base of deflection. Journal of Community Justice, 33(3), 5-10.
- McVicar, D., Moschion, J., & Van Ours, J. C. (2015). From substance use to homelessness or vice versa? Social Science and Medicine, 136, 89-98.
- Office of the Surgeon General (US). (2016). Facing Addiction in America: The Surgeon General's Report on Alcohol, Drugs, and Health. Washington (DC). Available from: https://www.ncbi.nlm.nih.gov/books/NBK424859/
- Ohio Department of Health. (2024). 2023 Ohio Unintentional Drug Overdose Report. https://content.govdelivery.com/attachments/OHIOGOVERNOR/2024/10/30/file_attachments/3052169/2023%2BUnintentional%2BDrug%2BOverdose%2BAnnual%2BReport_FINAL.pdf
- Ohio Department of Health. (2023). 2022 Ohio Unintentional Drug Overdose Report. https://odh.ohio.gov/wps/wcm/connect/gov/dea64cca-767c-4495-a75c-61b6f9d0f8fa/2022+Unintentional+Drug+Overdose+Annual+Report.pdf?MOD=AJPERES&CONVERT_TO=url&CACHEID=ROOTWORKSPACE.Z18_79GCH8013HMOA06A2E16IV2082-dea64cca-767c-4495-a75c-61b6f9d0f8fa-oNOoofn
- Ray, B., Richardson, N. J., Attaway, P. R., Smiley-McDonald, H. M., Davidson, P., & Kral, A. H. (2023). A national survey of law enforcement post-overdose response efforts. The American Journal of Drug and Alcohol Abuse, 49(2), 199-205.
- Redko, C., Rapp, R. C., & Carlson, R. G. (2006). Waiting time as a barrier to treatment entry: Perceptions of substance users. Journal of Drug Issues, 36(4), 831–852.
- Sahker, E., Pro, G., Poudyal, H., & Furukawa, T. A. (2024). Evaluating the substance use disorder treatment gap in the United States, 2016− 2019: A population health observational study. The American Journal on Addictions, 33(1), 36-47.
- Senthilkumar, R., Bailey, A., Moner, E., Parduhn, T., & Evans, E. A. (2024). Lessons Learned from Implementation of a Post-opioid Overdose Outreach Program in a Rural Massachusetts Community. Community Mental Health Journal, 60(3), 482-493.
- Substance Abuse and Mental Health Services Administration Center for Behavioral Health Statistics and Quality. (2015) Key substance use and mental health indicators in the United States: Results from the 2015 National Survey on Drug Use and Health.
- Substance Abuse and Mental Health Services Administration Center for Behavioral Health Statistics and Quality. (2015). Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health.
- Ulintz, A. J., McCloskey, R. J., Hammond, G. C., Parrish, M., Toliver, I., Sharafutdinova, A., & Lyons, M. S. (2024). RREACT: A mobile multidisciplinary response to overdose. Journal of Community Safety and Well-Being, 9(1).
- U.S. Census Bureau. (2023). Quick Facts: Hamilton County Ohio. https://www.census.gov/quickfacts/hamiltoncountyohio
ACKNOWLEDGEMENTS
The initial iteration of the Hamilton County Quick Response Team (HC-QRT) and its evaluation was funded by the Bureau of Justice Assistance (BJA) Comprehensive Opioid Abuse Site-Based Programs: System Level Diversion and Alternatives to Incarceration grant in 2017. Its expansion was funded by a 2020 BJA Comprehensive Opioid, Stimulant, & Substance Abuse Program (COSSAP) grant. Other activities deployed by the HC-QRT were also funded by National Institute of Health Healing Communities funding, a 2021 statewide COSSAP grant awarded to the Ohio Office of Criminal Justice Services, and a 2022 Substance Abuse and Mental Health Services Administration (SAMHSA) Grant to Expand Substance Abuse Treatment Capacity in Adult and Family Treatment Drug Courts.
The authors would like to recognize the hard work and effort of the QRT members at that time, and especially Captain Tom Fallon. We also want to recognize the commitment and coordination of the first QRT project manager, Emily May; the steadfast leadership and support of Hamilton County Commissioner Denise Driehaus; the support and guidance of the Association of Chiefs of Police; and the administrative support from Assistant County Administrator, Lisa Webb and colleagues from Cordata Healthcare Innovations—in particular, Kelly Firesheets and Laura Venerable.
TABLES
Table 1
OVERSDOSE RESPONSE |
(BJA COAP) PART TIME ➜10/1/17- 9/3/21 |
(BJA COSSAP) FULL TIME ➜ 10/1/21-9/30/24 |
BLACK/AFRICAN AMERICAN OUTREACH |
(STATEWIDE COSSAP) ➜ 10/1/20-9/30/24 |
JAIL-BASED NALOXONE DISTRIBUTION |
(NIH HEALING COMMUNITIES) ➜ 6/1/21-11/1/21 |
(BJA COSSAP) QRT EXPANSION ➜ 11/1/21-12/31/23 |
DRUG TREATMENT AND RECOVERY COURT PEER NAVIGATION |
(BJA COSSAP) QRT Expansion ➜ 7/1/21-10/1/22 |
(SAMHSA DRUG COURT)➜ 10/1/22-9/30/24 |
HOT SPOT OUTREACH |
(NIH HEALING COMMUNITIES) ➜ 9/1/21-6/30/22 |
(BJA COSSAP) HOPP ➜ 11/1/21-9/30/24 |
Timeline and Scope of HC-QRT Implementation
NOTE: Full-time overdose response and targeted outreach activities are currently still implemented, with the exception of jail-based Naloxone distribution
Table 2
Hamilton County Quick Response Team Logic Model
Inputs | Activities | Outputs | Outcomes | Impacts |
Funding
Core Team
Project Mgmt.
Advisory Board
Data Systems
Evaluation Team | Overdose response
Harm reduction distribution
Community outreach
Targeted outreach
Education
Peer support
Referrals/linkage to care | # people successfully engaged for overdose response
# people successfully engaged for targeted outreach
# Naloxone kits distributed
# Community outreach events
# miles traveled
# door knocks
# clients with ongoing successful engagement
% of successful engagements (of attempted contacts) | Short-Term Referrals to treatment
Connections to treatment
Long Term Decreased CJ involvement (pre-post)
Decreased overdose rates (pre-post)
Decreased service utilization (pre-post) | Improvement of community partnerships (macro)
Decreased calls for service for overdoses (macro)
Decreased overdose and overdose death rates (macro)
Decreased arrests for low-level drug-related offenses (macro) |
Table 3
Client Interaction Details, by Route of Engagement
Total # Unique Overdose Response Clients, Engagement Attempted Total # Unique Overdose Response Clients, Engagement Successful # unique clients with ongoing successful engagement % successful contacts (out of contact attempts) # unique clients referred or connected to treatment # Naloxone kits distributed | 2,643 1,127 223 (19.8%) 26.4% (n = 2,021/7,666) 441 452 |
Total # Unique Hot Spot/HOPP Clients, Engagement Attempted Total # Unique Hot Spot/HOPP Clients, Engagement Successful # unique clients with ongoing successful engagement % successful contacts (out of contact attempts) # unique clients referred or connected to treatment # Naloxone kits distributed | 2,514 2,410 123 (5.1%) 91% (n = 2,778/3,035) 75 2,624 |
Total # Unique African American Outreach Clients, Engagement Attempted Total # Unique African American Outreach Clients, Engagement Successful # unique clients with ongoing successful engagement % successful contacts (out of contact attempts) # unique clients referred or connected to treatment # Naloxone kits distributed | 732 573 39 (6.8%) 57% (n = 661/1,160) 39 456 |
Total # Unique Jail-Based Targeted Outreach Clients, Engagement Attempted Total # Unique Jail-Based Targeted Outreach Clients, Engagement Successful # unique clients with ongoing successful engagement % successful contacts (out of contact attempts) # unique clients referred or connected to treatment # Naloxone kits distributed | 216 201 2 (1%) 94.9% (n = 203/214) 5 217 |
Total # Unique DTRC Client, Engagement Attempted Total # Unique DTRC Client, Engagement Successful # unique clients with ongoing successful engagement % successful contacts (out of contact attempts) # unique clients referred or connected to treatment # Naloxone kits distributed | 1,142 1,125 673 (59%) 91% (n = 3510/3845) 55 72 |
Chart 1
Unique Clients Engaged, by Route of Engagement
AUTHORS
* Sarah M. Manchak, Ph.D.*
- University of Cincinnati School of Criminal Justice.
ORCID: 0000-0002-4703-4107
Requests to authors – Sarah M. Manchak, [email protected].
Sarah Light, M.S.
Madeline Lancaster, M.S.
- Institute of Behavioral Research, Texas Christian University. ORCID: -Unknown- | [email protected]
Bradley O’Guinn, M.S.
Meagan Guthrie, M.A.
- Hamilton County Ohio Office of Addiction Response. ORCID: -Unknown- | [email protected]
Cory Haberman, Ph.D.
WAIVER
- The ideas, concepts and conclusions set out in this research article do not represent an official position of the European Institute for Multidisciplinary Studies in Human Rights and Sciences - Knowmad Institut gemeinnützige UG (haftungsbeschränkt).
- The content of this article and of this Journal is dedicated to promoting science and research in the areas of sustainable development, human rights, special populations, drug policies, ethnobotany and new technologies. And it should not be interpreted as investment advice.
ACKNOWLEDGEMENT
Thanks to all those who have contributed to the production of this paper.
DONATE AND SUPPORT SCIENCE & HUMAN DIGNITY
IBAN: DE53 1705 2000 0940 0577 43 | BIC/SWIFT: WELADED1GZE |
TITULAR: Knowmad Institut gUG | BANCO: Sparkasse Barnim
http://bit.ly/ShareLoveKI
CC BY-NC 4.0 // 2025 - Knowmad Institut gemeinnützige UG (haftungsbeschränkt)
Contact: [email protected] | Register Nr. HRB 14178 FF (Frankfurt Oder)

This article is part of the Special Issue:
Deflection: A New Horizon for Police,
Public Health, and Community.
[1] Naloxone was not widely distributed until September 2020, when Ohio Governor Mike Dewine legalized widespread distribution of Naloxone by non-prescribing entities. Fentanyl test strips were not legalized until January 2023.
[2] For 46 individuals (.6%), the QRT engaged with another contact, such as a family member, case manager, or law enforcement, and did not have any further engagements with the referred individual directly. These 46 individuals were removed from subsequent analyses. Additionally, 16% of unique individuals targeted by the QRT were referred to the QRT 2 or more times, across routes of engagement over the seven-year period